That sharp twinge you feel when using your local stairs or that deep ache after walking from the MRT often signals knee osteoarthritis (OA).
This common ‘wear and tear’ condition can significantly impact your mobility, and it’s not just a simple feature of ageing.
Wondering if your knee pain is just a temporary ache or the first sign of osteoarthritis?
Understand the classic symptoms, when to see a specialist, and the difference between general arthritis and osteoarthritis.
Recognising the early signs of knee OA can help you seek treatment faster, which often leads to better outcomes. While symptoms vary, most patients report a gradual onset of these five common issues:
It’s easy to ignore knee pain, hoping it will go away. However, you should consider seeing a doctor if your pain is persistent (lasts for several weeks), interferes with your sleep, or stops you from doing daily activities.
Your first stop can be a General Practitioner (GP), who can provide an initial assessment. However, if the pain is severe, follows an injury, or doesn’t improve with basic rest, consulting an orthopaedic specialist is the most direct route. A specialist can perform a physical examination, order specific imaging like X-rays, and provide an accurate diagnosis and a tailored treatment plan.
This is a common point of confusion. Think of “arthritis” as a large family name for conditions that cause joint inflammation. There are over 100 different types.
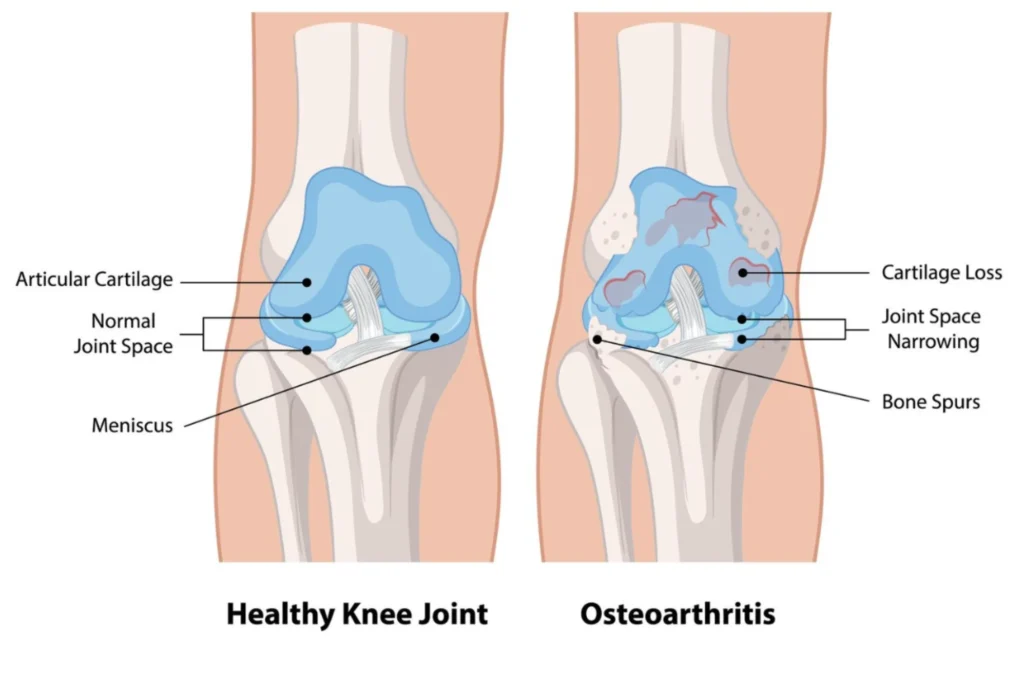
Osteoarthritis (OA) is the most common type, like the eldest child in the family. It is a degenerative, or “wear and tear,” disease where the protective cartilage that cushions the ends of your bones wears down over time.
Other types, like Rheumatoid Arthritis (RA), are autoimmune diseases, meaning your body’s own immune system mistakenly attacks the joint lining. Gout is another type caused by crystal deposits. A specialist can determine the exact type of arthritis you have, which is crucial as the treatment paths are very different.
Knee osteoarthritis is a progressive condition, but understanding its four distinct stages can empower you to seek the right treatment at the right time. We explain what happens at each stage, from minor wear to severe joint damage.
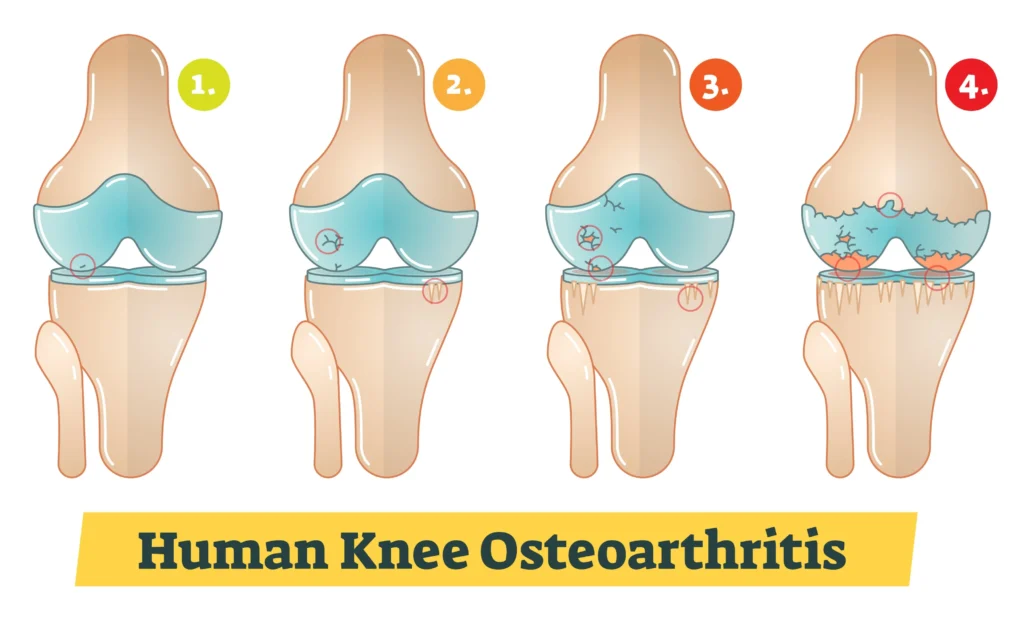
In Stage 1, there is very minor wear on the knee cartilage. Patients are often asymptomatic, meaning they feel no pain and notice no change in function.
An X-ray might show small bone spurs (osteophytes) growing, but the space between the bones is still normal.
At this stage, the focus is purely on prevention: maintaining a healthy weight and engaging in low-impact exercise to protect the joint.
This is the stage where most people first notice something is “off.” You might feel pain after a long walk, stiffness after sitting for a while, or tenderness when kneeling.
X-rays will still show a healthy joint space, but the bone spurs may be more defined.
This is the best time to intervene with non-surgical treatments, as lifestyle modifications and physiotherapy can make a substantial difference in slowing progression.
By Stage 3, the cartilage has obvious erosion, and the gap between the bones begins to narrow.
Patients typically experience pain during simple daily activities like walking or bending. Swelling is more frequent, and that “grating” sensation (crepitus) may become more pronounced.
Non-surgical treatments like injections are often introduced at this stage to manage the increasing pain and inflammation.
This is the most advanced stage of knee OA.
The protective cartilage is almost completely gone, leaving the bones to rub directly against each other. This “bone on bone” friction causes constant pain, severe stiffness, and a major loss of mobility. Joint deformity may also be visible.
At this point, non-surgical treatments may no longer provide relief, and your specialist will likely begin to discuss surgical options, such as a knee replacement, to restore your quality of life.
Many people think knee OA is just “getting old,” but the true knee osteoarthritis causes and treatment options are more complex.
Age is the single biggest risk factor for osteoarthritis. The simple fact is that our joint cartilage becomes more brittle and has less capacity to repair itself as we get older. However, age is not the only factor, and it’s not a guarantee you will develop OA.
Genetics also plays a part. Some people inherit genes that make them more susceptible to cartilage breakdown or having slight joint misalignments that increase wear. If your parents or siblings have OA, you may have a higher risk of developing it.
Excess weight is a major, and modifiable, risk factor.
For every 1 kg of extra weight you carry, your knees feel an extra 3-4 kg of pressure with every step.
Previous injuries, such as an ACL tear, meniscus tear, or a knee fracture, can dramatically increase your risk of developing post-traumatic osteoarthritis years later
Repetitive, high-impact stress (like from certain manual labour jobs) or sports that involve a lot of twisting and pounding (like football or marathon running) can accelerate the “wear and tear” process.
While you can’t change your genes or your age, you can control many of the other risk factors. The best “prevention” strategy is a proactive one.
Maintain a healthy body weight. This is the most effective thing you can do to protect your knees. Stay active with low-impact exercise. Movement is medicine. Activities like swimming, cycling, and strength training build the muscles around the knee, which act as shock absorbers.
Protect your joints. If you play sports, use proper technique and wear protective gear. If your job is physical, be mindful of your posture and lifting mechanics. Listen to your body and don’t “play through” the pain of an injury.

Surgery is not your only option. In fact, most knee osteoarthritis causes and treatment options are non-surgical. Discover the best exercises, dietary changes, and modern injections that can effectively manage pain and improve your mobility.
Yes, absolutely with a few caveats. Movement is crucial for knee health.
Walking helps lubricate the joint and strengthens the muscles that support it. The key is to choose low-impact activities.
While no diet can cure OA, certain foods can help manage inflammation. Focus on an anti-inflammatory diet, rich in Omega-3 fatty acids (found in fatty fish like salmon, mackerel, and sardines). Eating a colourful variety of fruits and vegetables provides antioxidants, which can also help.
Some patients find relief from supplements like Glucosamine and Chondroitin, though the medical evidence is mixed. It’s best to discuss any new supplements with your specialist to ensure they are right for you.
When pain persists, your specialist may recommend injections directly into the knee joint.
When non-surgical treatments no longer control the pain, it may be time to consider surgical options. We explain when a knee replacement is recommended and what the procedure involves, helping you understand the path to a pain-free life.
Many people manage their knee OA for their entire lives without ever needing surgery. The decision to have surgery is not based on your X-ray; it’s based on your quality of life. Your specialist will typically ask these questions:
If the answer is “yes” to these questions, then it’s time to have a conversation about surgery.
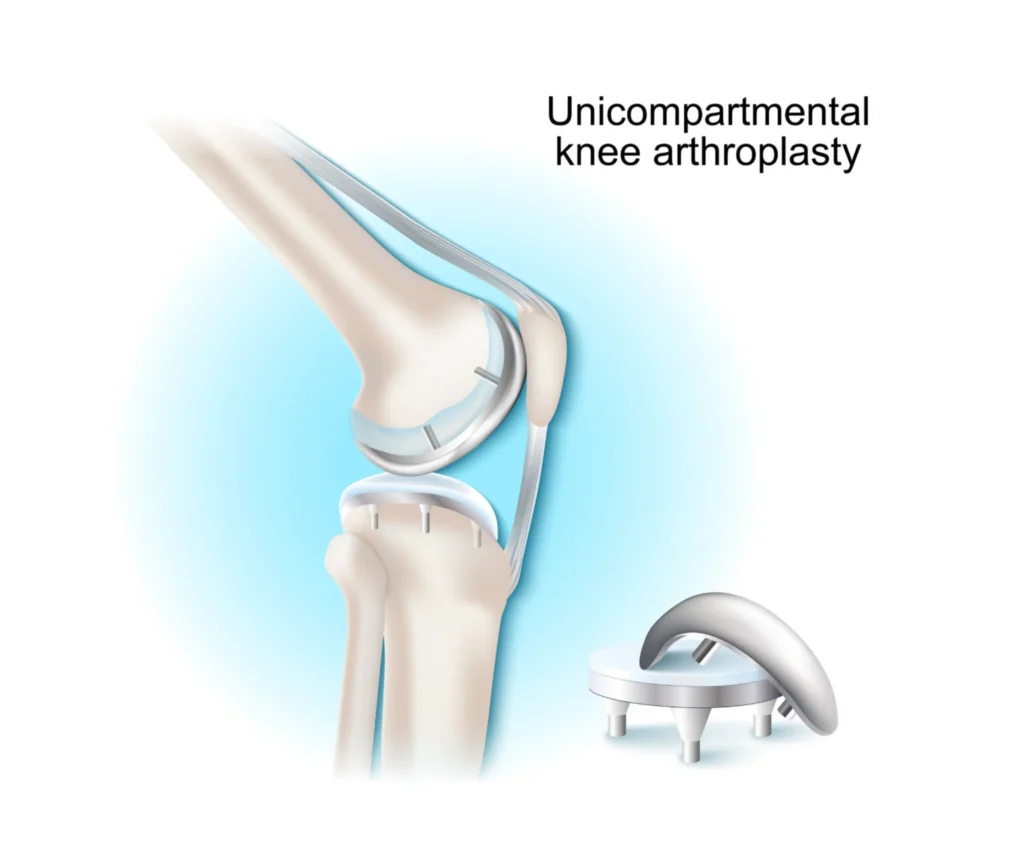
A total knee replacement is a highly successful and common procedure. Think of it as resurfacing a damaged road. The surgeon does not remove your entire knee. Instead, they remove only the damaged surfaces of the bone and cartilage at the end of your thigh bone (femur) and the top of your shin bone (tibia).
These surfaces are then “capped” with high-grade metal and plastic implants, creating a new, smooth-gliding joint.
You cannot reverse the underlying disease of osteoarthritis. However, you can absolutely recover from its painful and debilitating symptoms. A total knee replacement is designed to “cure” the pain and disability caused by the end-stage joint damage. After a successful surgery and a dedicated course of physiotherapy, the vast majority of patients return to an active, pain-free life.
Understanding the financial aspect of treatment is vital. Understand potential costs for managing knee osteoarthritis in Singapore, from initial consultations and MRIs to the use of MediSave and MediShield Life for surgery.
Disclaimer: All costs are estimates. Please consult our clinic for precise financial counselling.
Getting a diagnosis in the private system involves a few initial costs.
Specialist Consultation
An initial consultation with an orthopaedic specialist typically ranges from $150 to $250.
X-Ray
This is the first-line imaging test and is very affordable, usually costing between $80 and $150.
MRI Scan
If the specialist needs to see the soft tissues in high detail, an MRI may be ordered. This is more expensive, often ranging from $1,000 to $2,000 per joint.
In Singapore, knee treatment costs vary depending on whether care is non-surgical or surgical, and whether it is done in a private or subsidised setting.
Injections
Common options include corticosteroid, hyaluronic acid and PRP. In private clinics, corticosteroid injections typically cost around $500–$800 per knee.
Hyaluronic acid injections are usually $1,000–$1,800 per knee, while PRP injections range from $900 to $2,200 per knee, depending on the preparation and whether imaging guidance is used.
More advanced regenerative injections can cost $4,000 and above per knee.
Surgery
Minimally invasive keyhole procedures such as knee arthroscopy generally cost $6,000–$10,000+ in private hospitals.
Partial knee replacement typically ranges from $25,000–$45,000, while a total knee replacement in a private hospital usually costs $35,000–$50,000 or more.
Subsidised public hospital options are significantly lower but may involve longer waiting times.
Final out-of-pocket costs depend on hospital choice, surgeon fees, implants, length of stay, and how much can be offset by MediSave, MediShield Life or integrated insurance plans.
For more costly procedures like surgery, your Singapore healthcare financing plans are crucial.
Medisave
Medisave can be used to pay for hospitalisation and approved surgical procedures, up to specific withdrawal limits. For example, a complex knee replacement is claimable up to a certain amount from the Table of Surgical Procedures. Some outpatient treatments, like viscosupplementation, are also claimable up to $450 per year.
MediShield Life
This is a basic health insurance plan that helps pay for large hospital bills and selected costly outpatient treatments.
Integrated Shield Plans (IPs)
If you have an IP from a private insurer, it works on top of MediShield Life. These plans are what cover the bulk of the cost if you choose to be treated in a private hospital or an A/B1 ward in a public hospital. It is essential to check your specific plan for coverage, deductibles, and any co-payment required.
At The Orthopaedic and Pain Practice (TOPP), we employ targeted interventions such as corticosteroid injections for acute inflammation and viscosupplementation (hyaluronic acid) to improve joint lubrication. While they are a valuable resource for managing discomfort, their main purpose is to ease symptoms and create a comfortable window where you can better engage with the essential progression-slowing pillars of exercise and weight management.
Injections are fundamentally a tool for managing pain and reducing inflammation, not for reversing or structurally halting the progression of knee OA itself.

Dr Yong Ren brings extensive expertise to the field of minimally invasive orthopaedic procedures. His background includes specialist training in Switzerland, focusing on complex orthopaedic trauma and reconstruction, underscoring his capability in handling simple to highly complex joint issues.
Choosing us means you benefit from:
Dr Yong Ren’s practice prioritises the least invasive techniques, leading to smaller scars, less post-operative pain, and faster return to function.
We believe in treating the whole patient, not just the injury. This includes a full, multi-modal pathway from non-operative treatments (like physical therapy and injections) to the latest surgical techniques.
We provide clear, locally-relevant guidance on everything from the procedure itself to the intricacies of Medisave claimability and insurance processing in Singapore.
If you have been living with persistent pain, or if you have questions about your orthopaedic condition and wish to explore personalised, advanced treatment options, we encourage you to consult with Dr Yong Ren.
Take the first step toward a pain-free life with a $150 Knee Pain Consultation & X-ray.