A dislocated kneecap, or patellar dislocation, is a frightening and intensely painful injury. One moment your knee feels normal, and the next, your kneecap (patella) has visibly slipped out of its natural groove. This jarring event can happen during sports, from a fall, or even just from a sudden twist.
When a kneecap dislocation occurs, panic is a natural reaction. However, your actions in the first few minutes are crucial for minimising further damage. Do not attempt to force the kneecap back yourself; instead, focus on immobilisation, pain relief, and seeking immediate professional medical help.
While you wait for medical assistance, your focus should be on protecting the joint. The R.I.C.E. principle (Rest, Ice, Compression, Elevation) is a useful guide, but with some important modifications for a dislocation.
What Not to Do:
It can be tempting, especially from watching films or hearing stories, to try and force the kneecap back into its groove. This is an extremely dangerous idea. When the patella dislocates, it can chip the bone underneath or tear the delicate articular cartilage.
Forcibly “popping” it back in without a medical professional’s gentle technique and diagnostic imaging can:
This can turn a manageable injury that could have been treated non-surgically into one that definitively requires complex surgery.
The answer is simple: go immediately. A dislocated kneecap is a true orthopaedic emergency. Call for an ambulance or have someone drive you to the nearest A&E department in Singapore.
This is not a “wait and see” injury. You need a medical professional for two reasons:
Do not visit a GP or polyclinic first; they will simply refer you to an A&E.
While a dislocation is often visually obvious, its symptoms can sometimes be confused with other severe knee injuries. A correct diagnosis from a medical professional is the first step toward the right treatment plan. The doctor will use a physical examination and imaging to confirm the diagnosis and check for associated injuries.
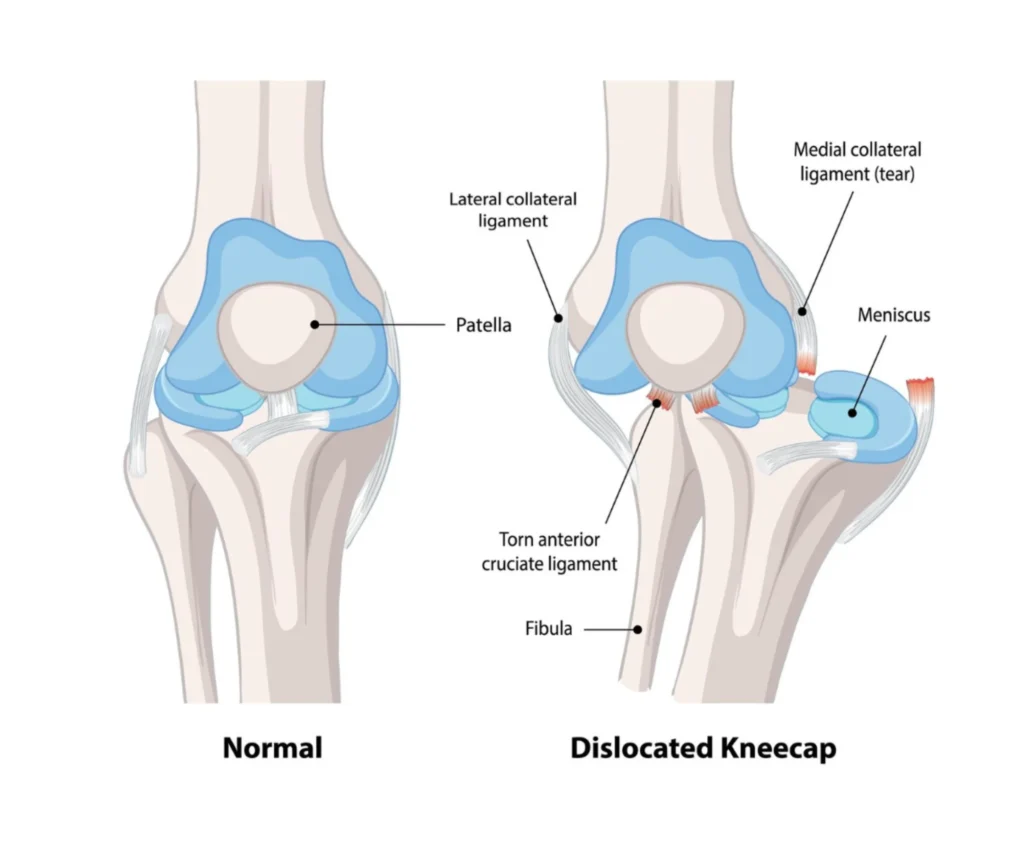
A severe sprain (like an ACL tear) and a patellar dislocation both cause extreme pain and swelling. However, a dislocation has one key distinguishing feature: a visible deformity.
Another condition is a patellar subluxation. This is a partial dislocation where the kneecap slips out of the groove but then pops back in on its own. This is still a serious injury that causes pain and a feeling of the knee “giving way,” and it requires specialist assessment.
The pain of an active kneecap dislocation is severe and sharp, often rated as a 9 or 10 out of 10 at the moment of injury. It is a distinct, sickening feeling.
You can also expect the following symptoms:
At the A&E, a doctor will first gently examine the knee, checking your pulse and nerve function in your foot to ensure no critical blood vessels were damaged.
The diagnostic process then follows two main steps:
Once a dislocation is confirmed, the first step is realignment, known as a “reduction.” After that, your treatment path will focus on healing and stabilisation. This path can be non-surgical, relying on physiotherapy, or may involve surgery to repair damage and prevent it from happening again.
A “closed reduction” is the medical term for the procedure used to put your kneecap back in place without surgery. “Closed” means no incision is made.
This procedure is typically performed in the A&E. The doctor will provide you with pain relief, and sometimes a sedative, to help your muscles relax. They will then gently and slowly straighten your leg while applying careful pressure to the outside of the patella, guiding it back into its groove (the trochlea). Patients often experience immediate and substantial pain relief the moment the kneecap is back in position. After the reduction, your leg will be placed in a brace or splint to keep it straight.
Yes, for most first-time patellar dislocations, the primary treatment is non-surgical. After the closed reduction, the treatment plan focuses on allowing the damaged ligaments to heal and strengthening the joint to prevent a recurrence.
This non-operative management involves:
Your orthopaedic specialist may recommend surgery if your case is more complex. Surgery is generally considered for:
The goal of surgery is stabilisation—to create a stable joint and prevent future dislocations.
Healthcare costs are a practical and necessary concern for patients in Singapore.
Understanding the financial landscape is part of the comprehensive care provided.
Getting a diagnosis in the private system involves a few initial costs.
Specialist Consultation
An initial consultation with an orthopaedic specialist typically ranges from $150 to $250.
X-Ray
This is the first-line imaging test and is very affordable, usually costing between $80 and $150.
MRI Scan
If the specialist needs to see the soft tissues in high detail, an MRI may be ordered. This is more expensive, often ranging from $1,000 to $2,000 per joint.
The cost of treating a kneecap dislocation varies widely.
It depends entirely on whether the treatment is non-surgical (involving an A&E visit, consultations, brace, and recurring physiotherapy sessions) or surgical (such as an MPFL reconstruction, which involves hospitalisation, surgeon, and implant fees).
The final bill is also determined by the choice between public (subsidised vs. unsubsidised wards) and private healthcare institutions.
Medisave
Medisave can be used to pay for hospitalisation and approved surgical procedures, up to specific withdrawal limits. For example, a complex knee replacement is claimable up to a certain amount from the Table of Surgical Procedures.
MediShield Life
This is a basic health insurance plan that helps pay for large hospital bills and selected costly outpatient treatments.
Integrated Shield Plans (IPs)
If you have an IP from a private insurer, it works on top of MediShield Life. These plans are what cover the bulk of the cost if you choose to be treated in a private hospital or an A/B1 ward in a public hospital. It is essential to check your specific plan for coverage, deductibles, and any co-payment required.

The initial pain and swelling will calm down within 1 to 2 weeks. The torn ligaments themselves need about 6 to 8 weeks to heal physically.
Physiotherapy is your single most crucial element. Skipping it is the biggest predictor of another dislocation. Its goals are straightforward: restore safe range of motion, aggressively strengthen the VMO (inner quad) and hip/glute muscles, and retrain your balance (proprioception).
Your brace is worn for the first 3 to 6 weeks to protect the healing ligaments by restricting movement.
Rehab progresses in phases, always cleared by your physio:
It usually comes down to three things:
If left dislocated, it’s an emergency causing severe disability. More often, if you skip physio, the ligaments heal loose. This leads to chronic instability and a high risk of recurrent dislocation with much less force. Each time it happens, it damages the cartilage, potentially leading to early osteoarthritis.
The mantra is consistency:

Dr Yong Ren brings extensive expertise to the field of minimally invasive orthopaedic procedures. His background includes specialist training in Switzerland, focusing on complex orthopaedic trauma and reconstruction, underscoring his capability in handling simple to highly complex joint issues.
Choosing us means you benefit from:
Dr Yong Ren’s practice prioritises the least invasive techniques, leading to smaller scars, less post-operative pain, and faster return to function.
We believe in treating the whole patient, not just the injury. This includes a full, multi-modal pathway from non-operative treatments (like physical therapy and injections) to the latest surgical techniques.
We provide clear, locally-relevant guidance on everything from the procedure itself to the intricacies of Medisave claimability and insurance processing in Singapore.
If you have been living with persistent pain, or if you have questions about your orthopaedic condition and wish to explore personalised, advanced treatment options, we encourage you to consult with Dr Yong Ren.
Take the first step toward a pain-free life with a $150 Knee Pain Consultation & X-ray.